Regulating the immune response in a targeted and localized way
Engineered immune cells may be able to tame inflammation
The immune system protects us from viruses, bacteria and other dangers. It distinguishes between the body's own cells and foreign cells, decides what is dangerous and adjusts the immune response accordingly. But when it is dysregulated, it can attack the body's own cells – as in the case of type 1 diabetes, where it destroys the insulin-producing beta cells of the pancreas. It can also reject foreign tissue in transplants. However, preventing this by suppressing the entire immune system carries serious health risks, such as increased susceptibility to infection and cancer.
The research team has now engineered regulatory immune cells that locally soothe an overreacting immune response. They specifically protect healthy body cells: they recognize them through their antigens and prevent T-killer cells from destroying them. The technology could be used to stop the body from rejecting transplanted organs and tissues. That way, patients would no longer need to take harsh immunosuppressant drugs.
The work was carried out at UC San Francisco (UCSF) with significant contributions from Matthias Hebrok, Professor of Applied Stem Cell and Organoid Systems at the Technical University of Munich (TUM), and Dr. Hasna Maachi, postdoctoral researcher at TUM and Helmholtz Munich. The study was published in the journal Science.
“This technology can put the immune system back into balance,” said Wendell Lim, PhD, UCSF professor of cellular and molecular pharmacology. “We see it as a potential platform for tackling all kinds of immune dysfunction."
To engineer the regulatory immune cells, the researchers are using the same type of cells as in CAR T-cell immunotherapies. For the latter, they are specifically engineered to target tumor cells. By contrast, the engineered regulatory immune cells are designed to protect healthy cells. The produce a combination of proteins that the researchers have found to be particularly effective for regulation: one has an anti-inflammatory effect, while the other scavenges pro-inflammatory substances. The cell system can be flexibly adapted for different applications.
The goal: to protect beta cells in type 1 diabetes
To test the application in type 1 diabetes, the researchers modified the cells to recognize and protect human beta cells. They introduced the engineered immune cells into mice that had received a transplant of human islet cells, modeling the treatment for type 1 diabetes. The experiments were successful: The transplanted beta cells that were protected by the engineered cells survived and continued to produce insulin. In contrast, transplanted cells without the protective engineered T cells were destroyed.
The authors envision a future in which organ transplant patients, or those with autoimmune diseases, receive therapies that only treat the specific regions of the body where the immune system is misbehaving, instead of shutting down the whole system. The new technology also could be used to finetune CAR T cell therapies for cancer, so these CAR T cells only attack tumors, and not healthy tissue.
Being able to modulate immune responses and to further optimize functional properties of stem cell derived tissues is central to developing long lasting stem cell therapies, a clear goal for organoid researchers at the new Center for Organoid Systems (COS) at TUM.
Nishith R. Reddy, Hasna Maachi, Yini Xiao, Milos S. Simic, Wei Yu, Yurie Tonai, Daniela A. Cabanillas, Ella Serrano-Wu, Philip T. Pauerstein, Whitney Tamaki, Greg M. Allen, Audrey V. Parent, Matthias Hebrok, Wendell A. Lim: Engineering synthetic suppressor T cells that execute locally targeted immunoprotective programs, Science (December 2024). DOI: 10.1126/science.adl4793
- Prof. Matthias Hebrok is Director of the new TUM Center for Organoidsystems (COS). Organoid research is a key research area at TUM. With the construction of the TUM Center for Organoid Systems (COS) at the Garching Research Center, TUM is developing a facility unlike any in Europe. It will utilize TUM’s status as a technical university with its own university clinic to transfer this ultramodern technology into medical-clinical applications.
- Prof. Matthias Hebrok conducts research at the Munich Institute of Biomedical Engineering (MIBE), an Integrative Research Institute at TUM. At MIBE, researchers specializing in medicine, the natural sciences, engineering, and computer science join forces to develop new methods for preventing, diagnosing or treating diseases. The activities cover the entire development process – from the study of basic scientific principles through to their application in new medical devices, medicines and software.
- The professorship of Applied Stem Cell and Organoid Systems is part of the TUM School of Medicine and Health.
- The project was funded by: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Valhalla Foundation
Technical University of Munich
Corporate Communications Center
- Carolin Lerch
- presse@tum.de
- Teamwebsite
Contacts to this article:
Prof. Dr. Matthias Hebrok
Technical University of Munich
Professorship of Applied Stem Cell and Organoid Systems
matthias.hebrok@tum.de

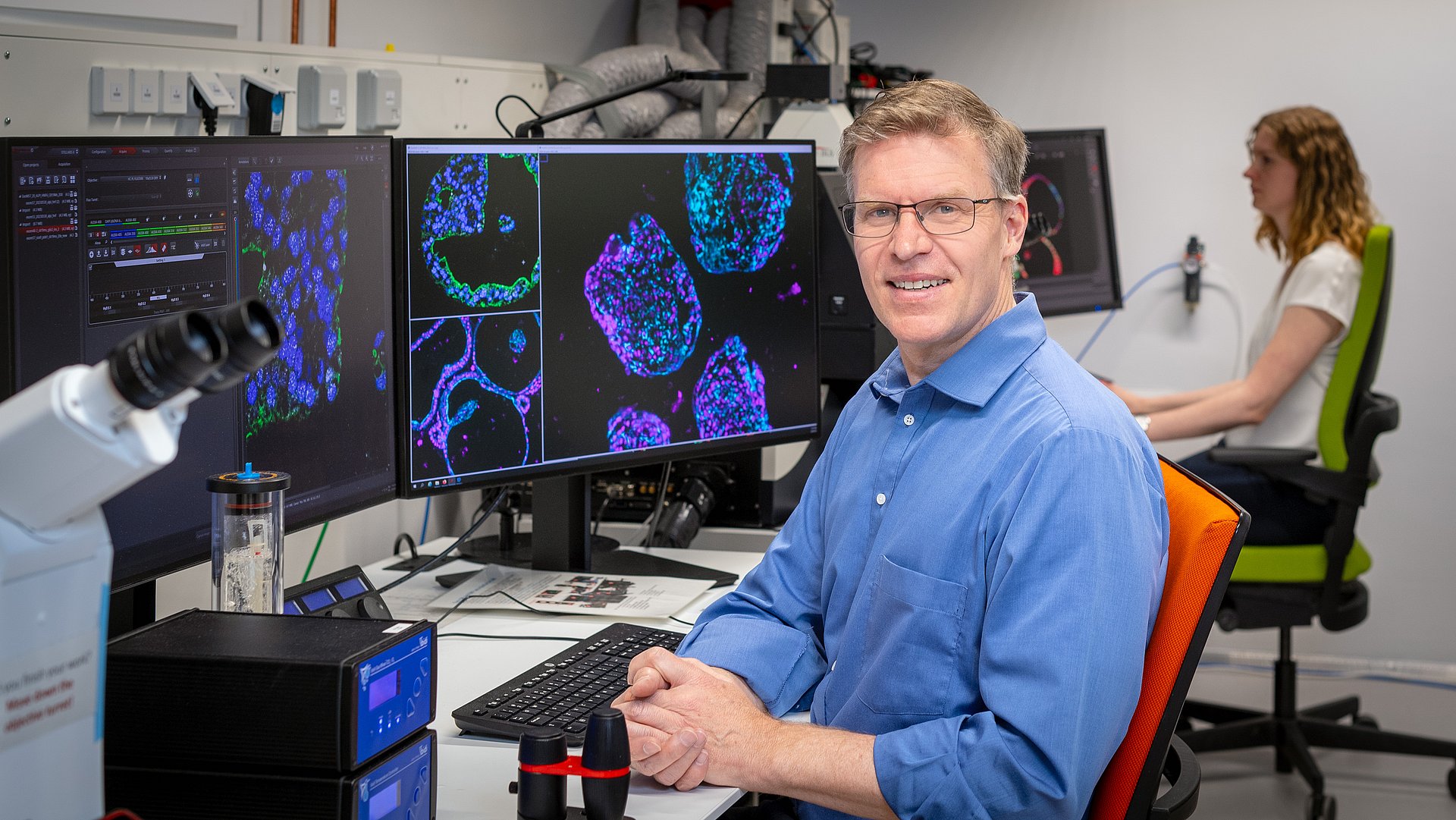
![[Translate to English:] [Translate to English:] NewIn: Matthias Hebrok.](/fileadmin/user_upload_87/_processed_/7/2/csm_20230530_Hebrok_AH_759056_7f158f61c6.jpg)
